Forums » News and Announcements
Hemostatic agents for prehospital hemorrhage control
-
Hemorrhage is the leading cause of preventable death in combat trauma and the secondary cause of death in civilian trauma. A significant number of deaths due to hemorrhage occur before and in the first hour after hospital arrival. A literature search was performed through PubMed, Scopus, and Institute of Scientific Information databases for English language articles using terms relating to hemostatic agents, prehospital, battlefield or combat dressings, and prehospital hemostatic resuscitation, followed by cross-reference searching. Abstracts were screened to determine relevance and whether appropriate further review of the original articles was warranted. Based on these findings, this paper provides a review of a variety of hemostatic agents ranging from clinically approved products for human use to newly developed concepts with great potential for use in prehospital settings. These hemostatic agents can be administered either systemically or locally to stop bleeding through different mechanisms of action. Comparisons of current hemostatic products and further directions for prehospital hemorrhage control are also discussed.To get more news about шлемы, you can visit rusuntacmed.com.ru official website.
A broad PubMed search without restriction to publication date for English language articles relating to hemostatic, battlefield or combat dressings and/or prehospital hemostatic resuscitation was performed and followed by cross-reference searching. The search terms were as follows: prehospital or pre-hospital or battlefield or combat or military, trauma* or wound or bleeding, hemorrhag* or haemorrhag*, or hemostatic agent or dressing. The specific product names and active agents (e.g., Combat Gauze: a kaolin-impregnated nonwoven gauze made by Z-Medica Corporation; HemCon, ChitoGauze, and ChitoFlex: chitosan-based dressings made by HemCon Medical Technologies; Celox: granules and gauze made from more than one type of chitosan and manufactured by Medtrade Products Ltd.; XStat produced by Revmedx, and chitosan, dried plasma, fibrinogen concentrate, fibrin sealant, tranexamic acid, platelet) were also used as keywords in the search.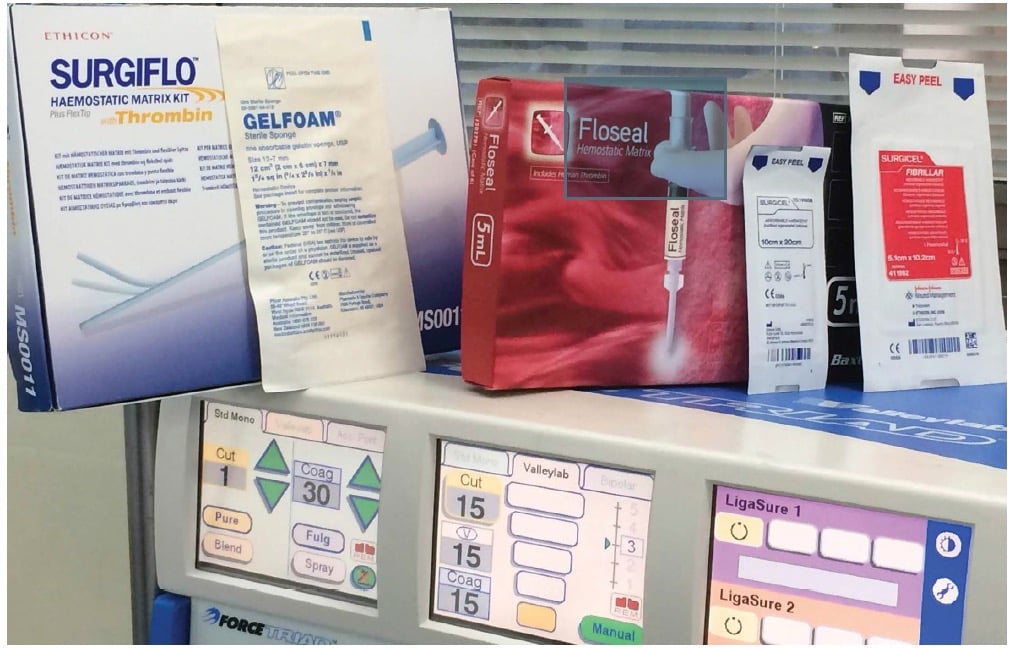
Abstracts were screened to determine relevance and when appropriate further review of the original articles was warranted. Additional publications were selected from the cross-references listed in the original papers and from the cited articles, and additional searches were performed through Medline, Scopus and Institute of Scientific Information databases for those topics with limited findings from PubMed.
The search was primarily focused on human studies of the hemostatic agents already operationally deployed for control of severe/active bleeding or deemed to be applicable in both military and civilian prehospital settings. Some animal studies that employed lethal injury models for comparison of combat and prehospital hemostatic agents were included given the limited number of comparative studies in humans. All human studies were eligible for inclusion, regardless of study design (i.e., trials, case reports and reviews). The focus of this review was on hemostatic agents and thus hemostatic devices (e.g., tourniquets) were excluded.
It should be noted that the literature search, screening and assessment were not conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) protocol [32]. As the search was performed by a single author, there may be bias for the assessment of relevance of articles for inclusion. The review was limited to English language papers with dominance of local hemostatic agents and several dressings.
A recent study suggests that 82% of the deaths occur because of uncontrolled bleeding out of total preventable combat deaths [4]. Moreover, mortality due to excessive bleeding contributes to about one-third of the total traumatic deaths in the world [5]. Laceration or fracture of the scalp contributes to 60% of the total traumatic haemorrhage incidences [6]. Uncontrolled bleeding compromises the balance between the demand and supply of the tissue oxygen at the injury site which can ultimately lead to cardiac arrest [7]. If efforts are made to stop bleeding, death would be preventable. Conventionally, cotton gauze is used with pressure to stop bleeding as the first line of treatment, which may not be always successful and has many limitations. The ideal characteristics of the haemostatic dressing include the ability to stop bleeding quickly, absorb blood, simple application and removal, and it should be porous enough to allow oxygen transfer to the wound site [8-9]. Apart from these properties, a haemostatic dressing should have antimicrobial properties and be non-allergic in nature as it is directly exposed to the open bleeding wound [9]. Today’s need is a topical, simple, and advanced haemostat to stop bleeding rapidly before the patient reaches the hospital [10]. In recent years, several haemostatic agents, effective through a different mechanism of actions, have been developed and studied to efficiently control severe bleeding as compared to conventional cotton gauze [11].
