Forums » News and Announcements
The use of Haemostatic Agents
-
The use of Haemostatic Agents does not impact the rate of hemorrhagic complications
Hemostatic agents(HAs) have gained increasing popularity as interventions to improve perioperative haemostasis and diminish the need for allogeneic red cell transfusion(PBT) despite a paucity of data supporting the practice. The aim of the current study is to examine the efficacy of HAs in reducing the rate of hemorrhagic complications during partial nephrectomy(PN). Data on 657 patients, who underwent elective PN between 2004–2013, were analyzed. The impact of HAs and SURGICEL was evaluated by comparing four sequential groups of patients: Group1 = Sutures alone, Group2 = sutures and HA, Group3 = sutures and SURGICEL, Group4 = both HA and SURGICEL. Complications included post-operative urinary leak(UL), PBT rate, delayed bleeding and post-operative renal failure. Results showed that the use of HAs did not engender a statistically significant difference in overall complications rate. Specifically, the addition of HAs did not reduce the rate of PBT, delayed bleeding or UL. Further analysis revealed that patients who received SURGICEL had significantly higher PBT rate and higher prevalence of UL cases. Addition of HAs to SURGICEL had no effect on the rate of these complications. In the current study, the use of HAs during open and laparoscopic PN did not reduce the rate of negative outcomes. Adequate suture renorrhaphy may be sufficient to prevent hemorrhagic complications.To get more news about IFAK kit, you can visit rusuntacmed.com official website.
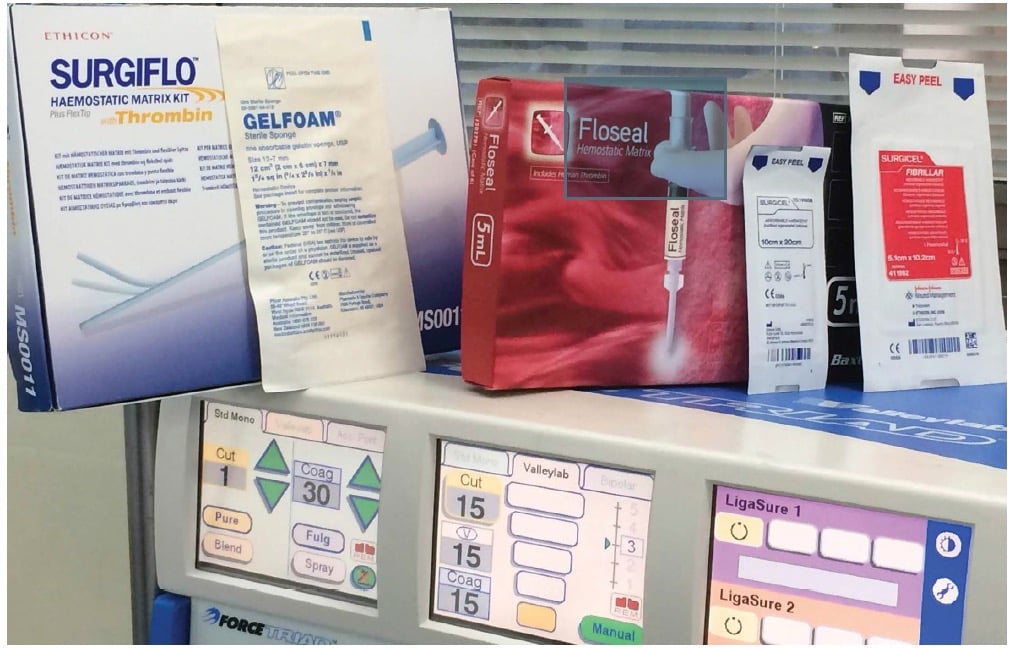
In recent years, partial nephrectomy (PN), and specifically laparoscopic PN (LPN) has become the standard of care in the management of selected renal lesions1. Initially, LPN was proffered only in the case of a small, peripheral, exophytic tumor. However, with increasing experience, the application of LPN has extended to tumors invading more deeply into the renal parenchyma up to the collecting system or renal sinus2,3. Nevertheless, as laparoscopic surgeons approach more difficult tumors, the complexity of tumors requiring Open PN (OPN) is even further magnified. In both approaches, the excision of such deeply infiltrating tumors routinely necessitates division of major intrarenal vessels and precise entry into the collecting system to ensure an adequate margin of resection. Such resections are therefore associated with significant risks of bleeding and urinary leak3.Despite the relatively low incidences of hemorrhagic complications requiring transfusion after PN, it remains one of the most serious complications4. With many reports suggesting that allogeneic blood transfusion is associated with an adverse outcome5,6,7, several attempts have been made to reduce the risk of bleeding. In the past decades, a wide variety of haemostatic agents (HAs) has been developed as surgical tools, in order to reduce the rate of such complications. Different tissue adhesives (also called glues) have been used to assist in haemostasis and collecting system closure during open and laparoscopic PN2,8,9,10,11,12. Yet, despite the growing clinical application of HA during PN, there is little data regarding their cost-effectiveness in preventing major complications13. In this study, we present an analysis of the effectiveness of using HAs and glues in laparoscopic and open PN.
A total of 657 consecutive patients underwent PN at our institution between 2004 and 2013. All operations were performed in the same surgical environment (four surgeons operating in one medical center). Patient demographics and surgical details were collected retrospectively, following an approval given by the Sheba Medical Center Institutional Review Board (IRB)/Ethics (Helsinki) Committee, in accordance with relevant guidelines and regulations. The need for informed consent was waived by our IRB. All patients were considered for a comparative study, and four groups were defined on the basis of the method of haemostasis used during the procedure. Group 1 = renorrhaphy was completed using sutures alone in 147 patients (22.4%); Group 2 = both sutures and HA were used in 26 patients (3.9%); group 3 = sutures and SURGICEL (Ethicon, Somerville, NJ, USA), without HA in 183 (27.8%) patients; and group 4 = sutures, HA and SURGICEL in 301 (45.8%) patients.
